Every morning Kathy Reagan Young steps out of the shower in her Virginia Beach home, towels off, dons a pair of protective goggles and stands nine inches from a light box the size of a small space heater. Young presses a button, and the box’s bulbs begin to glow a ghostly purple. She briefly bathes her torso in the ultraviolet rays coming from the bulbs, four minutes per side. Then she goes about her day.
That Young can have an ordinary day is remarkable. In 2008 she was diagnosed with multiple sclerosis (MS), a terrible malady in which the body’s own immune system attacks the sheaths that insulate the nerves, destroying them bit by bit. Symptoms begin with weakness, spasms, vision and speech problems, intense fatigue, and what Young calls “cog fog”—chronic low-grade cognitive impairment. Flare-ups can lead to periods of motor-control loss and paralysis. Young, an advocate for MS patients and creator of a popular podcast, has suffered through many such episodes. But things improved with the arrival of her light box.
Ultraviolet (UV) light boxes, which emit only a narrow bandwidth of light that is not linked to skin cancer, have been used for years in the treatment of psoriasis. Young got a prescription from her doctor, and the box was sent to her by a medical-device company called Cytokind that is hoping to expand such use to MS and other autoimmune diseases and was looking for some practical patient feedback. She tried out the device and gave them some pointers: make it smaller and easier to hold because MS often makes your hands go numb, and build in timed reminders to overcome the cog fog. Then, to her surprise, she found that her fatigue disappeared a few months after she started using it.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
For years Young had been forced to rest in bed many times a day, but that stopped with what she calls her UV-fueled rebirth. “I was in a meeting, and someone said to me, ‘Wow, you seem like you’re pretty high energy!’” Young says. “And I guess I hadn’t really thought about it. And then two days later my daughter said to me, ‘Mom, what are you on?’ I think we were all a little surprised by how quickly and definitively it happened.” Her MS Disease Activity (MSDA) score, which rates MS severity based on the levels of key inflammatory molecules in the blood, was a 1 out of 10, the best possible score, and it has stayed low for more than a year. MS has no cure, and Young still suffers from transient pain and tingling, but the return of her vitality has made it all more bearable. “It’s incredible,” she says. “My friends used to invite me to things, and I’d say yes, but I always canceled because I was wiped out. Well, not anymore.”
Young is one of the first people in the U.S. to test UV phototherapy as an MS treatment, but she may be at the forefront of a revolution in how we think about light and a huge class of diseases. Autoimmune diseases such as MS and type 1 diabetes occur when our natural defenses—our immune systems—viciously turn against our own bodies and organs. These illnesses are estimated to affect more than 350 million people worldwide. Treatments have been elusive.
Although only a handful of clinical trials for MS light therapy have been conducted in people, evidence from a number of medical studies now shows that UV light, the highest-energy part of the solar spectrum that reaches Earth’s surface, has a surprising ability to calm an immune system that has bolted out of control. The new studies offer tantalizing hints that UV therapy might also work for other autoimmune diseases such as type 1 diabetes, rheumatoid arthritis, Crohn’s disease and colitis. All are more common in people who get very little sun exposure, as are maladies such as Alzheimer’s and cardiovascular disease that appear to have some immune system and inflammatory connections.
Now scientists are hoping to decipher the pathways through which UV light causes the immune system to back down from its alarm state. They are tracking the way molecules in the skin such as urocanic acid and lumisterol—which can affect immune system activity—respond to a shot of photons by triggering a cascade of signals that reach every organ in the body. Advocates say this work might lead to a blockbuster drug, an Ozempic for autoimmunity.
“UV light calms inflammation in the skin, the nervous system, the pancreas and the gut. Its potential is not fully realized.” —Prue Hart, Kids Research Institute Australia
Scientists not involved in the light research are more cautious, but they agree that something important is going on. “UV light therapy holds promise,” says Annette Langer-Gould, an MS researcher and neurologist at Kaiser Permanente in Los Angeles. But she would like to see rigorous and larger trials on various diseases and a better understanding of the mechanism.
That kind of confirmation could also solve a mystery that has vexed scientists for more than a century: Why do people living in lower-light environments have such high rates of disease?
The trail that led scientists to the discovery of UV light’s beneficial effects began with the confirmation of its dangers. In 1974 pioneering researcher Margaret L. Kripke (who would go on to found the department of immunology at MD Anderson Cancer Center in Texas) discovered that she could induce tumors in the skin of mice by exposing the rodents to UV light. But those tumors failed to grow when transferred to the skin of a different mouse. The new host’s immune system quickly eliminated them. Ten times she tried, and 10 times the tumors were squelched. When she suppressed the new host’s immune system with drugs, however, the tumors took hold. “That was the key!” she later recalled.
But why was the tumor able to grow in the original irradiated mouse? Was the UV light that had induced it also somehow suppressing the mouse’s natural immune response? In a series of experiments, Kripke determined that UV radiation was indeed a double whammy. Not only did it damage DNA in skin cells and trigger mutations that could lead to cancer, but it also suppressed the immune system’s surveillance of the skin, preventing that system from killing any budding cancers. This finding was a breakthrough in our understanding of how skin cancer develops, but it also seemed nonsensical from an evolutionary perspective. How could it possibly be beneficial for our immune system to relax in the presence of a common carcinogen?
It turns out that immune cells in our skin evolved to walk a fine line. As our primary interface with the outer world, the skin is barraged with potential stressors: heat, cold, wounds, bug bites, mysterious microbes of all kinds. For the first million years that our nonape ancestors spent under tropical African skies, solar radiation was the most common stressor of all. “It’s a challenge to the body,” says Prue Hart, an immunologist at the Kids Research Institute Australia who has been studying the effects of sunlight on immunity for more than 30 years. “It’s the most important environmental insult we have. We evolved to cope with it.”
But if the immune system had reacted to every kiss of sunlight with a full-throated attack, Hart says, we’d have lived in a constant state of inflammation, beset by rashes, hives and cutaneous autoimmune disorders. Instead the system learned to hold its fire.
In prehistoric times, this was the right approach. The damage was usually minor, the skin repaired itself, life went on. The trade-off—especially now that people live long enough for slow-growing tumors to get big and spread to other parts of the body—is that every so often a skin cancer sneaks through. One fascinating confirmation of this idea is polymorphic light eruption (PLE), a common disorder in which patients’ immune systems are not suppressed by sunlight. PLE sufferers develop itchy rashes and plaques after sun exposure, but they are less likely to develop skin cancer.
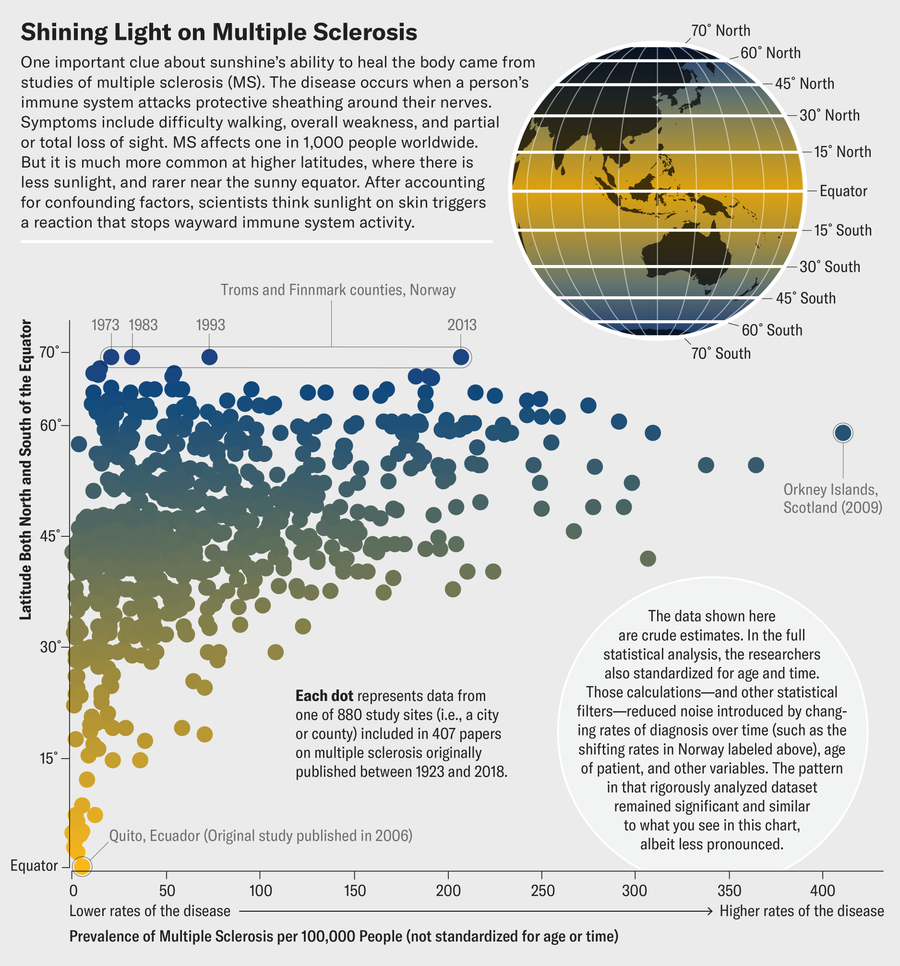
Jen Christiansen; Source: “Latitude Continues to Be Significantly Associated with the Prevalence of Multiple Sclerosis: An Updated Meta-Analysis,” by Steve Simpson, Jr., et al., in Journal of Neurology, Neurosurgery & Psychiatry, Vol. 90, No. 11; November 2019 (data)
The discovery of UV light’s powerful impact on our immune responses launched a brand-new discipline: photoimmunology. Early investigators in this field, such as Kripke, focused on the negative effects of immunosuppression. But they soon found some upsides as well. For example, it finally explained something doctors had noticed for centuries: sunlight soothed psoriasis, a skin condition marked by painful, itchy scales. With the discovery that psoriasis was an autoimmune disease in which the immune system flays the body’s own skin cells, it at last made sense. UV light—whether from the sun or a lamp—improved psoriasis by tamping down the inflammatory response.
Remarkably, the effect wasn’t just local. Shining light on one patch of inflamed skin could reduce symptoms on other patches. Even more curious, people with psoriasis often suffer from other autoimmune conditions, and sometimes the phototherapy improved their other symptoms as well.
As photoimmunologists probed deeper into the mechanisms, they began to wonder whether the body’s response to UV light was more than skin-deep. In the laboratory, they exposed mice to UV radiation and saw their entire immune systems pivot to anti-inflammatory states. In mice with autoimmune diseases, it improved their health. The researchers began comparing notes with epidemiologists, who were documenting signs of the same thing in human populations.
For more than a century scientists have noticed that many diseases, especially autoimmune and cardiovascular conditions, follow a latitude gradient. Once other confounding factors such as diet, exercise and socioeconomics are accounted for, rates of these diseases rise with latitude. All kinds of causes have been suggested—climate, diet, cosmic rays, something in the water—but nothing fit.
In 1940 a physician at the Medical College of Virginia named Frank Apperly showed that American states and Canadian provinces receiving more solar radiation had higher rates of skin cancer mortality but lower rates of cancer mortality overall. Skin cancer was known to be caused by sunlight, but Apperly suggested that something about the sun was also conferring protection against internal cancers. He didn’t know what, but in 1980 Johns Hopkins University epidemiologists Frank and Cedric Garland, two brothers who were analyzing maps of cancer incidence produced as part of the government-led “war on cancer,” noticed a strong north-south gradient for colon cancer rates and suggested in a hugely influential paper in the International Journal of Epidemiology that vitamin D was responsible.
Until then, vitamin D had been known mostly as the micronutrient that prevented rickets. It is produced in the skin with the aid of sunlight, and it helps to deliver calcium to bones, making them resistant to fractures. The Garlands suggested that it might do a lot more than that, and indeed, everywhere scientists looked they discovered an inverse correlation between vitamin D levels and the risk of dozens of diseases, including breast cancer, high blood pressure, diabetes, heart attack, stroke, dementia, depression, and several autoimmune disorders.
Thus began the vitamin D era. Doctors around the world recommended supplementation with this new wonder drug, and they still do for people who are seriously deficient in the substance. But as recently chronicled in this magazine, rigorous clinical trials have shown that extra D supplementation—using the vitamin as a treatment—doesn’t help with any of these diseases. The maladies afflict people who take supplements and people who don’t, in equal measure. Most of us get enough D from just a little sunlight or from our diets: fortified dairy products are good sources, for instance, as are fatty fish such as salmon. Whatever sunshine is doing to prevent myriad ailments, it’s a lot more complicated than getting the skin to produce a little vitamin D.
The disease with the most dramatic latitude gradient is MS. Prevalence rates are close to zero near the equator and increase by 3.64 cases on average per 100,000 people for each degree of latitude, reaching well over 100 cases per 100,000 people in northern Europe and North America. The gradient exists worldwide and has been growing stronger over time. It even shows up within individual countries, including France, the U.K., Sweden, New Zealand, Canada and the U.S.

Kathy Reagan Young, who has multiple sclerosis, uses ultraviolet rays from a light box for a few minutes every morning. Since she began treatment, her symptoms have eased notably.
Some of the best data comes from Australia, which is one of the only countries to boast a wide range of latitudes, a relatively homogeneous population and a national health-care system with good recordkeeping. A 1981 study found that rates of MS rose from 12 per 100,000 people in tropical Townsville (19 degrees latitude) to 21 in Brisbane (27 degrees), 37 in Newcastle (33 degrees), and a whopping 76 per 100,000 people in Hobart (43 degrees). The latitude connection was reinforced in the early 2000s, when a study of various environmental factors that might contribute to MS onset found rates several times higher in Australia’s higher latitudes.
At the time, says Robyn Lucas, an epidemiologist at the Australian National University who is one of the leaders of the study, many scientists assumed a lack of vitamin D at the higher latitudes was responsible. “Vitamin D was the flavor of the day. Vitamin D was cancer. Vitamin D was cardiovascular disease,” she says. “Vitamin D was autoimmune disease. Vitamin D was everything. And we just thought, ‘Yeah, vitamin D.’”
But in 2010 Lucas read a study showing that UV treatments protected mice against MS without affecting their vitamin D levels. Mice are not always good stand-ins for people, but it was enough to make Lucas curious. “I’d just done the analysis of the vitamin D, and then this paper came out, and I thought, ‘Okay, let’s have a look at that,’” she says. “So I went back to our data and actually found a much stronger effect for sun exposure.”
Since then, Lucas and others have found signs of sunlight’s preventive effect on MS everywhere they’ve looked. People with the most sun damage on the back of the hand—a particularly accurate reflection of lifetime sun exposure—have just one-third the rate of MS compared with those with less. And kids who spent less than 30 minutes a day outside had twice the risk of MS compared with those who spent up to one hour outside and about five times the risk of those who averaged more than an hour outside.
Notably, observational studies like these cannot prove causation. There could be other explanations for the patterns. Perhaps people suffering the earliest symptoms of MS spend more time indoors because they’re not feeling well. Maybe something else about high-latitude locations contributes to MS. So epidemiologists looked for other supporting evidence, and they found plenty. Even within the same region, MS relapse rates follow a seasonal cycle—higher in winter, when sun is scarce—and incidence rates correspond closely to birth month, being highest in people who experienced winter during their first trimester of gestation, when the brain and immune system are developing.
Additional support came from a small clinical trial by Hart. She recruited 20 patients with clinically isolated syndrome, an early-stage version of MS that eventually leads to full MS. Half the subjects received eight weeks of treatment with a narrowband-UV light box similar to the one Kathy Reagan Young uses, undergoing three sessions per week with each session lasting just a few minutes. The other half didn’t get light therapy. Within a week of the first treatment, levels of inflammatory proteins in the UV group’s blood dropped, and they stayed lower even after the UV sessions ended. Three months after the beginning of the trial, the UV group’s disease-severity scores had fallen 13 percent, whereas the control group’s had risen 14 percent. These scores correlated with the subjects’ self-reported fatigue. A year after the sessions, all the subjects who didn’t get UV therapy had developed full-blown MS, but 30 percent of the UV group had been spared.
The fact that the effect lasted for months after the initial UV treatment was intriguing. Immune cells are constantly being produced in the bone marrow, and they don’t last that long, so the UV hadn’t just suppressed the immune cells in circulation; it had reset the system to a more tolerant state. “I think UV is part of our innate immune training,” Hart says. “It reprograms subsets of innate immune cells as they evolve out of the bone marrow. They’re less inflammatory and more regulatory.”
The idea is similar to recent research showing that early exposure to small amounts of allergens can condition the immune system and prevent a hyperactive response later on. “You get this rebalancing,” Hart says. “UV light calms inflammation in the skin. But it also then calms inflammation in the central nervous system. It’ll calm inflammation in the pancreas and the gut. So I think it’s not fully realized the potential it has to be a controller of body homeostasis.”
The implications go well beyond MS or even autoimmune diseases. In recent years researchers have learned that many other chronic conditions also have an inflammatory component. Cardiovascular disease is caused in part by immune cells attacking and damaging the walls of blood vessels. Alzheimer’s disease is connected to low-grade, smoldering inflammation in the brain. Arthritis, asthma, allergies, diabetes and even depression are thought to have inflammatory components. Something about the modern, indoor, overly hygienic lifestyle may cause our immune systems to lose their healthy set points.
Sun-exposure effects have also been found in some other autoimmune conditions, such as type 1 diabetes, in which the immune system attacks the pancreas, disrupting insulin production. The rate of this disease is threefold higher in southern Australia than in northern Australia. In the U.S., prevalence is lowest in fall babies, who gestated over the summer. But the difference is most pronounced in northern regions and smallest in sunny spots such as Hawaii and southern California.
Taken together, Lucas says, these findings start to make a very convincing case. “We’ve now shown it in pediatric MS, we’ve shown it in Crohn’s disease, we’ve shown it in type 1 diabetes,” she says. “There’s a consistency of evidence across autoimmune diseases that have a similar immunopathology.”
Given this consistency of evidence, what should we do about it? Although some scientists have argued for increased sun exposure for people at high risk of an autoimmune disease, few health-care providers would ever be comfortable recommending a known carcinogen to their patients. The holy grail, in terms of widespread acceptance, would be to uncover the mysterious molecular pathway through which the skin tells the immune system to relax and then turn it into a biologic—a medication isolated from natural organisms. “What is the Ozempic for autoimmunity?” asks Cytokind co-founder John MacMahon. “Where is it going to come from? Is there something in that photoimmune cascade that can be identified?”

Young strolls in the sunshine near her Virginia home. Her ultraviolet therapy has let her resume her daily activities and minimized many difficulties and pains created by her multiple sclerosis.
“We don’t know what the golden molecule is; we just know it’s not vitamin D,” Hart says. “So you take a step back and give UV, which gives the skin a chance to make whatever it is.” But a pill would be better than a light box as a treatment, MacMahon says. “People prefer pills,” he says, and doctors prefer prescribing pills, and pharmaceutical companies definitely prefer making pills.
The problem in finding “whatever it is” is that when you do shine UV light on the skin and take a peek to see what it makes, you discover a microscopic pharmacopeia. In addition to vitamin D, the skin produces melatonin, serotonin, endorphins, endocannabinoids, cortisol, oxytocin, leptin, nitric oxide, cis-urocanic acid, itaconate, lumisterol, tachysterol, and a dozen other vitamin D–like compounds that don’t even have names yet.
Most of these molecules are hormones or neurotransmitters, and that should come as no surprise. Although many people tend to think of the skin as nothing but a barrier, it’s the largest organ in the body and a vital pole of the neuroendocrine system, in constant conversation with the body and brain about how to tune the system to maintain health. It’s also a major site for the immune system, stocked with body-defending—or body-attacking, if they go haywire—T cells, macrophages, neutrophils, cytokines, antimicrobial peptides, and other key players.
The way UV light stirs this many-flavored stew is both elegant and complex. For example, the body stocks the skin with a precursor to vitamin D called 7-dehydrocholesterol. When the molecule is hit with the right amount of UV energy, one of its bonds breaks, allowing its atoms to flip to a new configuration. But when hit with more UV energy, it flips to a different configuration known as lumisterol, which has been found in the blood in higher concentrations than vitamin D and has known anti-inflammatory and antitumor effects. The skin takes advantage of the bond-breaking power of UV radiation to produce multiple molecules, including cis-urocanic acid and nitric oxide, which lowers blood pressure and reduces inflammation throughout the body.
Other skin cells respond to sunlight by increasing production of pro-opiomelanocortin, a protein that is then cleaved by enzymes into three essential molecules: beta-endorphin, a neurotransmitter that causes feelings of well-being and reduces stress hormones; adrenocorticotropic hormone, which triggers the release of cortisol, a steroid that regulates stress and suppresses inflammation; and the alpha form of melanocyte-stimulating hormone, which repairs damaged cells, inhibits proinflammatory molecules and produces melanin to darken the skin.
Immunologist Scott Byrne of the University of Sydney recently discovered six novel lipids—all with names like acylcarnitine and phosphatidylethanolamine, and no, that will not be on the final test—that are produced by the skin in response to UV light and sent down to the lymph nodes under the skin, where various immune cells meet and exchange information. There they signal T cells—the powerful immune warriors that get out of control in people with MS and attack the nervous system—to stay put and stop proliferating. This pathway is separate from the one that suppresses cancer surveillance in the skin, which means it holds the promise of harnessing the good of UV radiation without the bad.
No one fully understands how this biological pachinko game sorts itself out as all these cells and signals bounce off one another, so the quest for the golden molecule will not be completed tomorrow—and is unlikely to have a simple resolution. “Isn’t it naive to think one molecule is going to solve all the health conditions controlled by UV?” Hart says. A single cause would certainly be convenient, “but we evolved under the sun for millions of years. It’s probably multiple.”
Likewise, phototherapy itself is unlikely to deliver all the benefits of full-spectrum sunlight, but it doesn’t have to. Its safety, simplicity and affordability mean all it has to do is deliver some benefit. “Phototherapy is so cheap relative to biologics,” Hart says. “It’s almost a no-brainer as an adjunct treatment for all these inflammatory autoimmune diseases.”
That fact alone has drawn the interest of insurance companies. A UV light box costs about $2,000, whereas adalimumab (Humira), a leading biologic drug for various autoimmune diseases, lists for $80,000 a year and must be taken for life. Inspired by that math, along with clinical trials showing phototherapy to be as effective as some medications with fewer side effects, Kaiser Permanente provided 2,200 of its psoriasis patients with free at-home UV light boxes as an experiment. Fewer than a third of them went on to use biologics. Kaiser Permanente now lists at-home UV as a recommended treatment for psoriasis.
But Langer-Gould, the MS expert at Kaiser Permanente, says that although she’d be interested to see whether the light boxes the insurer uses for psoriasis would be helpful for MS, it’s too soon to make that leap. “Hart’s data are very encouraging,” she says. “But the current evidence is not enough to conclude a definitive treatment effect and recommend widespread use. We need at least one more study.” That study would have to be a clinical trial large enough to show a significant improvement in patients’ underlying conditions. Cytokind is currently pursuing such a study, but the results are probably still years away.
In the meantime, the flexibility of phototherapy will allow Young and other converts to fashion their own healing protocols—independence that becomes all the more precious when you have a debilitating disease. “MS robs you of so much,” Young says. “You can’t get out of bed, can’t go to work, can’t clean your house, can’t get your groceries. You’ve got to find rides just to go to the doctor.” For now, at least, she has traded all that for busy days of weight training, yoga, charity work, live chats, guided meditations—and a few minutes of UV light every morning. “It’s just so empowering,” she says. “To find a treatment that lets you actually take care of yourself is kind of amazing.”
Reporting for this piece was supported by the Nova Institute for Health.









