August 15, 2024
5 min read
Eating Disorders Can Strike Anyone
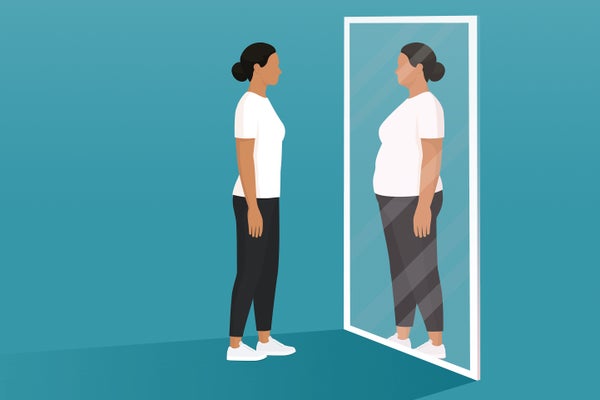
Misconceptions that eating disorders mostly afflict white, affluent, young females have led to disparities in the treatment of these deadly diseases
“I still don’t trust my parents’ ability to feed me,” confessed Sofia after I asked what she was most anxious about, nearing discharge after two months on an inpatient eating disorders unit where I worked as a psychiatry resident. The 14-year-old girl was brought to the pediatrician by her parents, worried about her eating. They learned that Sofia (whose name has been changed for her privacy) had lost 30 pounds over three months—she was eating only one piece of fruit a day in the weeks leading up to her admission. She could barely walk home from school, her menses ceased, her hair fell out in clumps, and her heart rate dangerously slowed.
But Sofia was not the patient that people often envision with an eating disorder. Her family was Spanish-speaking and had emigrated from Peru. Her confession contained both her fears about losing control of her eating as well as real concern for her life after leaving the hospital.
Her deeply caring family struggled with family sessions during her inpatient treatment, complicated by the need for interpreters, a prescribed inpatient diet that differed from the meals typically eaten at home, and a hesitancy to ask questions of the health care team. While Sofia was successfully restored to a healthy weight at discharge from the hospital, finding appropriate outpatient treatment presented yet another challenge. Family-based treatment is a standardized outpatient therapy, which aims to restore adolescent patients to a healthy weight with the support of their parents; the therapy consists of three phases where the parents begin with most of the feeding responsibility, and the patient gradually gains more autonomy as they become renourished. It is the gold standard for adolescent outpatient therapy. However, Medicaid did not fully cover most of these programs, and finding one with a Spanish-speaking therapist was even rarer. Despite a social worker’s efforts, Sofia was wait-listed for a family treatment program with a Spanish-speaking provider who offered sliding-scale payment.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Sofia’s case highlights the disconnect between who develops an eating disorder and the stereotypes portrayed in popular TV shows and movies like 13 Reasons Why and Black Swan. Media-fueled misconceptions about eating disorders predominantly affecting white, affluent, young females have resulted in disparities: underdiagnosis, lack of treatment access and limited understanding of eating disorders, leading to poorer outcomes.
Eating disorders include anorexia nervosa, bulimia nervosa, binge-eating disorder and avoidant/restrictive food intake disorder. These diseases have grave physical consequences, such as heart arrhythmias, and psychiatric ones, such as depression and suicidality. They are also on the rise, likely related to social isolation in the wake of the COVID-19 pandemic and increased social media use. With a 5 percent mortality rate, anorexia nervosa is one of the deadliest psychiatric illnesses in the world. From Taylor Swift to Princess Diana to Jane Fonda, eating disorders are not a new phenomenon.
Despite what people may think, eating disorders are equally prevalent across socioeconomic status, racial and ethnic groups, affecting approximately 9 percent of females and 4 percent of males. Emerging data even suggest individuals with multiple marginalized identities may be at higher risk. In one study of over 120,000 people, lower-income individuals were 27 percent more likely to have an eating disorder compared with those of higher income. This research also found that 52 percent of bisexual men and 52 percent of lesbian women of Latinx ethnicity and lower socioeconomic status screened positive for an eating disorder.
Our relationship to food is complex. Likewise, ethnicity, the stress of cultural assimilation, Western beauty standards, racial discrimination and trauma shape the prevalence of eating disorders.
Low-income patients and patients of color are also more likely to have missed diagnoses and not receive treatment. In a statewide study of California’s Medicaid-insured youth, the annual eating disorder prevalence was 0.2 percent compared with the 5 percent national prevalence estimate. That highlights the stark underdiagnosis and limited public funding of treatment for eating disorders. Moreover, when compared with national prevalence rates of eating disorders, health care professionals missed around 50 percent of diagnoses in Black youth in the U.S. Diagnostic bias likely underpins this underdiagnosis: presented with identical eating disorder symptoms, clinicians are more likely to diagnose a white patient than a Black patient. Diagnosis and treatment are inextricably linked; correctly identifying patients is the first step in effective treatment. Additionally, training non–mental health care providers in eating disorders is critical; if pediatricians or social workers don’t know the warning signs, they won’t see them.
Like accurate diagnosis, health care access determines treatment. In the U.S. treatment access is inextricably linked to how much money you have, where you live, who holds political office, stigma and blatant discrimination. One study published in 2018 found that Latinx youth with eating disorders were less likely to use mental health services compared to non-Latinx youth. Affluence was directly correlated with understanding a need for treatment (52 percent more likely) and receiving treatment (89 percent more likely) compared with low-income students in the study. Altogether, specialist services appear less accessible to low-income patients. For instance, eating disorder specialty services concentrate in more affluent areas and many offer services only to those with private health care. Outpatient behavioral health services often deny patients on Medicaid, as shown by Sofia’s inability to access family-based treatment. Given these diagnostic and treatment inequities, disparities in disease outcomes are inevitable. Early diagnosis and treatment are the best indicators of recovery and decreases in illness and death.
So how can we change these disparities? Fundamentally, we can’t know what we don’t study. The lack of inclusive research sustains stereotypes and fuels diagnostic bias. In the majority of eating disorder research, information on socioeconomic status is inconsistent and sexual orientation is absent. Although more studies report race and ethnicity data, funding and recruitment are often limiting factors. There is a seismic difference between collecting data and finding ways to proactively recruit diverse, representative participants. Most people included in eating disorder research are still white women. Few men, people of color, and even fewer gender-diverse individuals have been studied.
Ultimately, diversifying research will enable better treatment. In health care, increased evidence justifies increased investment, a bootstrap effect that helps explain why eating disorder treatment remains desperately underfunded. The heightened risk of patients with multiple minority identities necessitates investigation, including how the intersectional experience of having multiple identities and facing discrimination may affect the disease.
I am thankful that the institution where I work provides full weight restoration treatment at no cost and doesn’t need to rely on insurance companies, which would have likely resulted in Sofia being discharged at a much lower weight to outpatient care. However, free specialty care is a rare occurrence in the U.S. And even with quality inpatient treatment, I wish I had more outpatient treatment options to offer Sofia, and couldn’t help feeling like the system and we, as an extension of the system, were failing her on discharge. Eating disorders can affect anyone, and changing the narrative is critical in the endeavor for more equitable treatment. To ensure equal treatment for people like Sofia, we must raise awareness about the spectrum of individuals affected by eating disorders and address these biases in research, funding and patient care.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.








